Improving medication adherence
And why solutions are a way off
With the turning of the calendar year, I found myself part of the OptumRx specialty pharmacy. As someone who’s written a few pieces about Optum and how I believe their approach to consolidation is likely to remake American healthcare in a bureaucratic, expensive way, I was expecting to encounter a frustrating process. But unlike previous experiences I’ve had with specialty pharmacies, Optum filled my prescription quickly and without a prior authorization fight (I have to give credit where it’s due; I still don’t think the company should be running American healthcare).
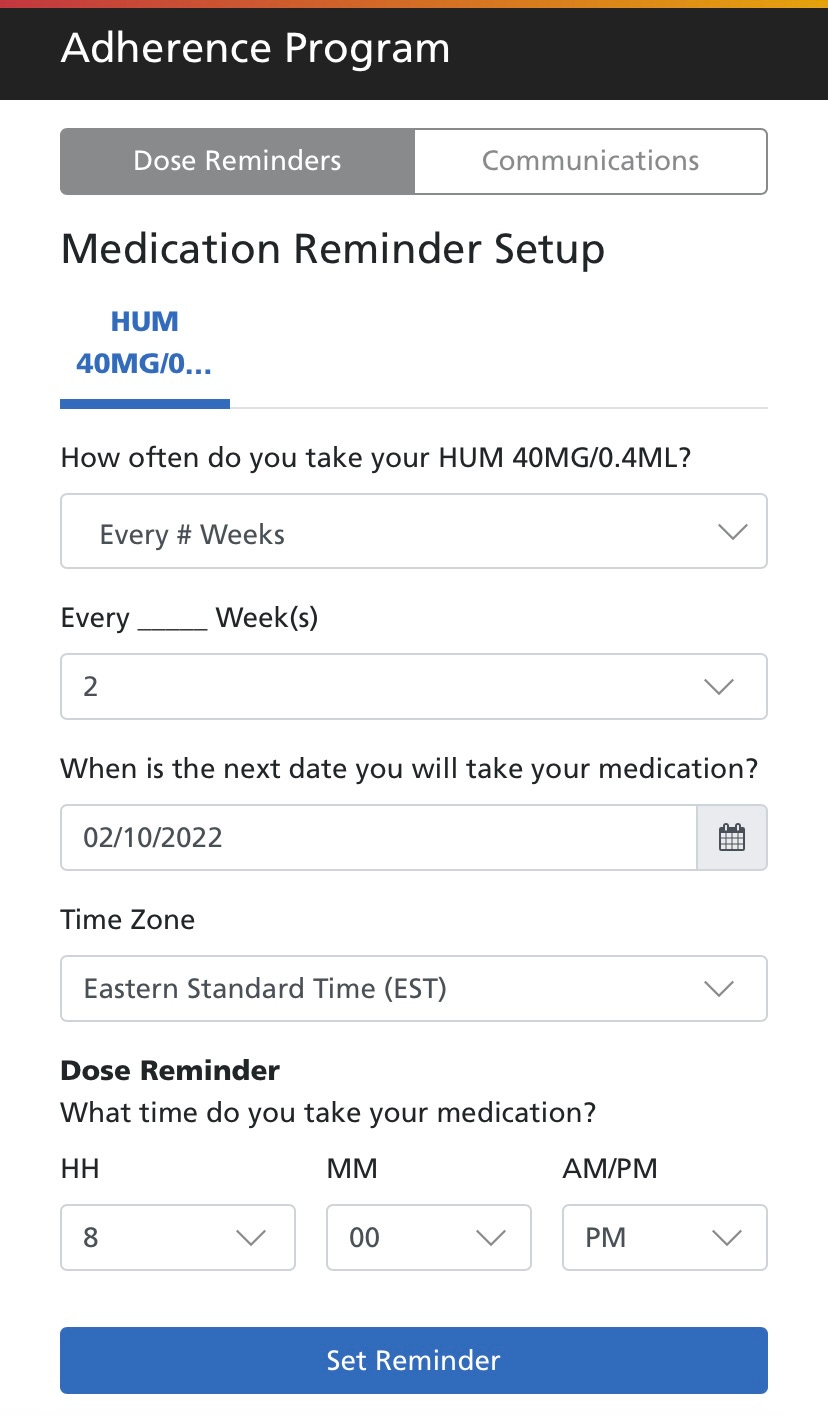
The most interesting part of the process, though, was how the company encourages medication adherence. After I received my medication, Optum sent me a text with a link to an opt-in medication reminder.
Granted, the bar is extremely low. *I* could probably figure out how to code something like this using online tutorials, and I was a history of health major. But when the bar is on the floor, something like this is pretty exciting.
It also got me thinking about the concept of medication adherence, and how it ties to value-based care.
Medication adherence
The reasons people have for not taking their medication are manifold. The medication might be too expensive, the pharmacy too far away, the side effects too onerous, the label too blurry (or the patient’s eyesight too poor), the person’s living situation might not be conducive to adherence, and so on.
A doctor once told me about a patient they had who was experiencing medication side effects. “Walk me through how you take your medication,” the doctor said, only to watch, shocked, as the patient took 11 pills instead of the prescribed 1 per day. “Well, it says ‘once per day,’” the Spanish-speaking patient said.
It will not surprise you to learn that medication non-adherence negatively affects public health. It’s estimated to cost between $100-289 billion (which is a laughably large range, I know) and cause more than 100,000 deaths per year. As many as 1 in 5 U.S. prescriptions are never filled, and of the 80% that are filled, about 50% are taken incorrectly.
Approaches to improving adherence
Because of how impactful medication non-adherence can be, quality metrics for Medicare value-based care programs, including the star rating system for Medicare Advantage programs and the ACO model, measure medication adherence. This is measured both indirectly (how well is a patient’s condition under control?), and, for patients with Medicare Part D, directly (is the patient refilling their prescription appropriately?).
Because of the financial implications for compliance, there’s a growing market of companies offering medication adherence solutions. (Try googling ‘medication adherence’ and check out the sponsored ads.) In 2017, Flare Capital Partners’ Dan Gebremedhin and Kara Warner created a helpful matrix to organize these companies:
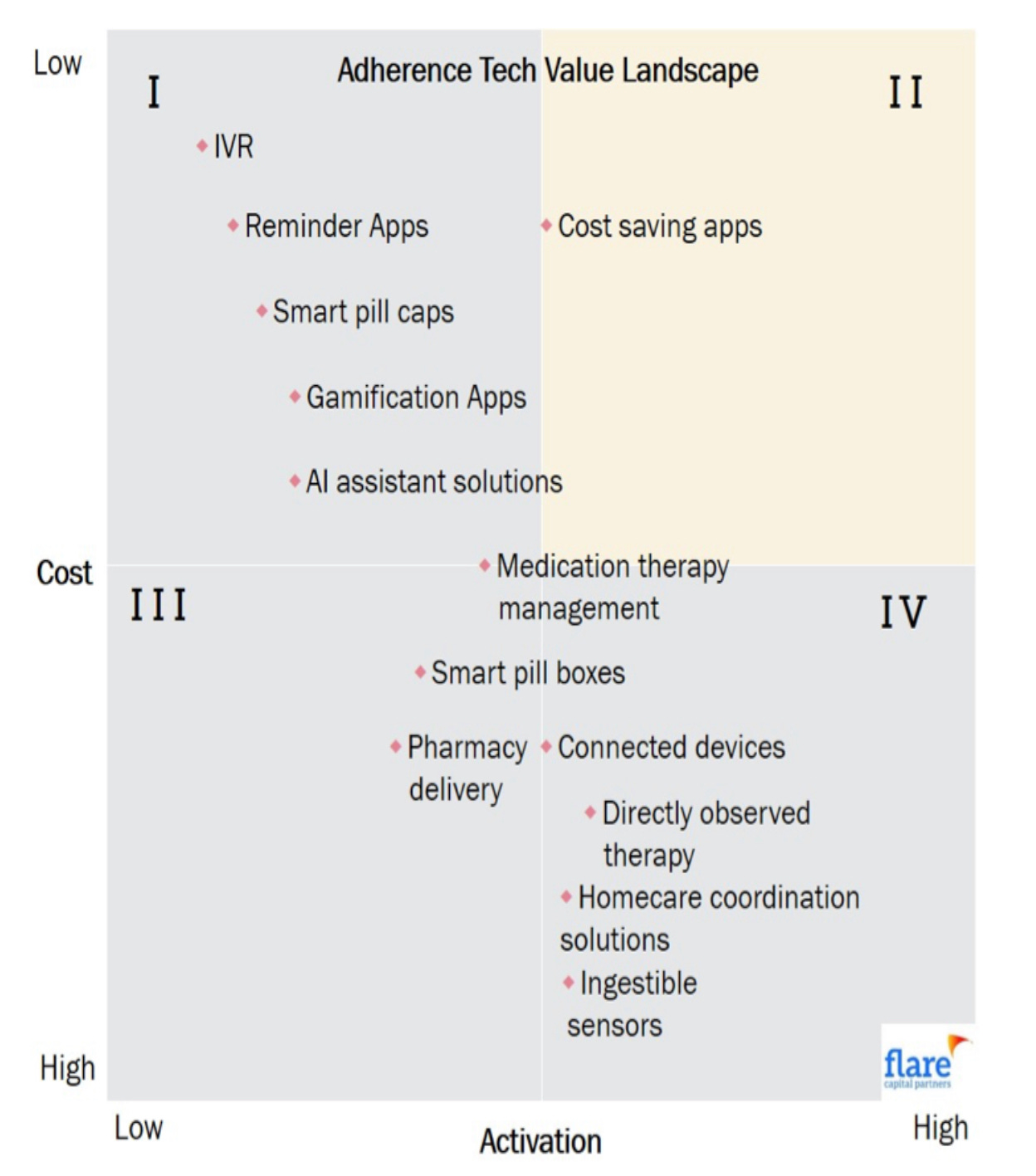
Despite the number and breadth of companies, though, uptake by providers with value-based contracts and insurers has been relatively slow. In their excellent review of the topic, Gebremedhin and Warner argue that:
First, payers are hesitant to adopt solutions that require upfront reimbursement and do not have proven savings. Startups who present potential “cost savings” figures tend not to be true cost utility analyses that factor in the cost of deployment of the intervention. Second, payers insure broad populations that have variable medication adherence needs. When faced with blanket PMPM vendor contracts, payers doubt the cost effectiveness of paying for services not utilized by segments of the population. Finally, some industry veterans will float a cynical maxim that increased medication adherence is a slippery slope that drives utilization and increases drug costs, creating a negative incentive for payers.
Hospitals
Notwithstanding their lukewarm interest in purchasing solutions, hospitals have tried a variety of internal programs to increase medication compliance. In a 2016 Deloitte report, the authors specifically cite two examples of hospital pilot programs: First, the University of Pennsylvania’s HeartStrong program, which used electronic pill bottles with sensors gauging whether the bottle had been opened each day. Second, a pilot at the University of Massachusetts to test digital pills that tracked when the pill was ingested.
These programs sounded exciting but were less than successful. A 2017 review of HeartStrong in JAMA found that the program did not significantly decrease rehospitalization, medication adherence, or cost. The digital pill model is still a possible avenue—there have since been studies on digital pill technology demonstrating that it’s feasible and relatively simple for patients to use—but it has yet to see wide adoption.
Other pilots, including one at UMass Amherst, are using a multidimensional coaching model. This kind of close relationship-building is a very promising one—but as I wrote about a year ago upon news that the Camden Coalition (which took a similar approach) failed to see statistically significant outcomes, providers taking this approach have yet to figure out how to scale it successfully.
Retail pharmacies
Some retail pharmacies, incented by the margin they make from prescription refills, have also started experimenting with increasing medication compliance. In 2019, Walgreens began hiring health outcomes pharmacists to use refill information to see which patients were likely to have adherence issues. But while retail pharmacies might be successful at increasing refill rates (CVS in particular is known for semi-shady and potentially dangerous approaches), that doesn’t necessarily translate to the patient actually taking the medication as directed.
Pharmaceutical manufacturers
Pharmaceutical manufacturers—especially those of high-price, high-margin specialty drugs—are also interested in medication adherence. At least to date, the manufacturers have relied on pretty low-tech methods, including hiring nurses to call patients and ask if they have questions, or partnering with specialty pharmacies like OptumRx to send text message reminders (as I received).
Conclusion
Although no one entity has figured out how to meaningfully improve medication compliance at scale, every entity that’s experimenting is doing so because of incentives from value-based care. And so, while value-based care has yet to fully deliver on its promises of higher-quality/lower-cost, a future with riskier payment models, bigger swings, and more partnerships might just see meaningful action on the medication adherence front.
This information shouldn’t be taken as investment advice (obviously), and the opinions expressed are entirely my own, not representative of my employer or anyone else.