Vaccinating people under 40
A challenge made more difficult by the express medical economy
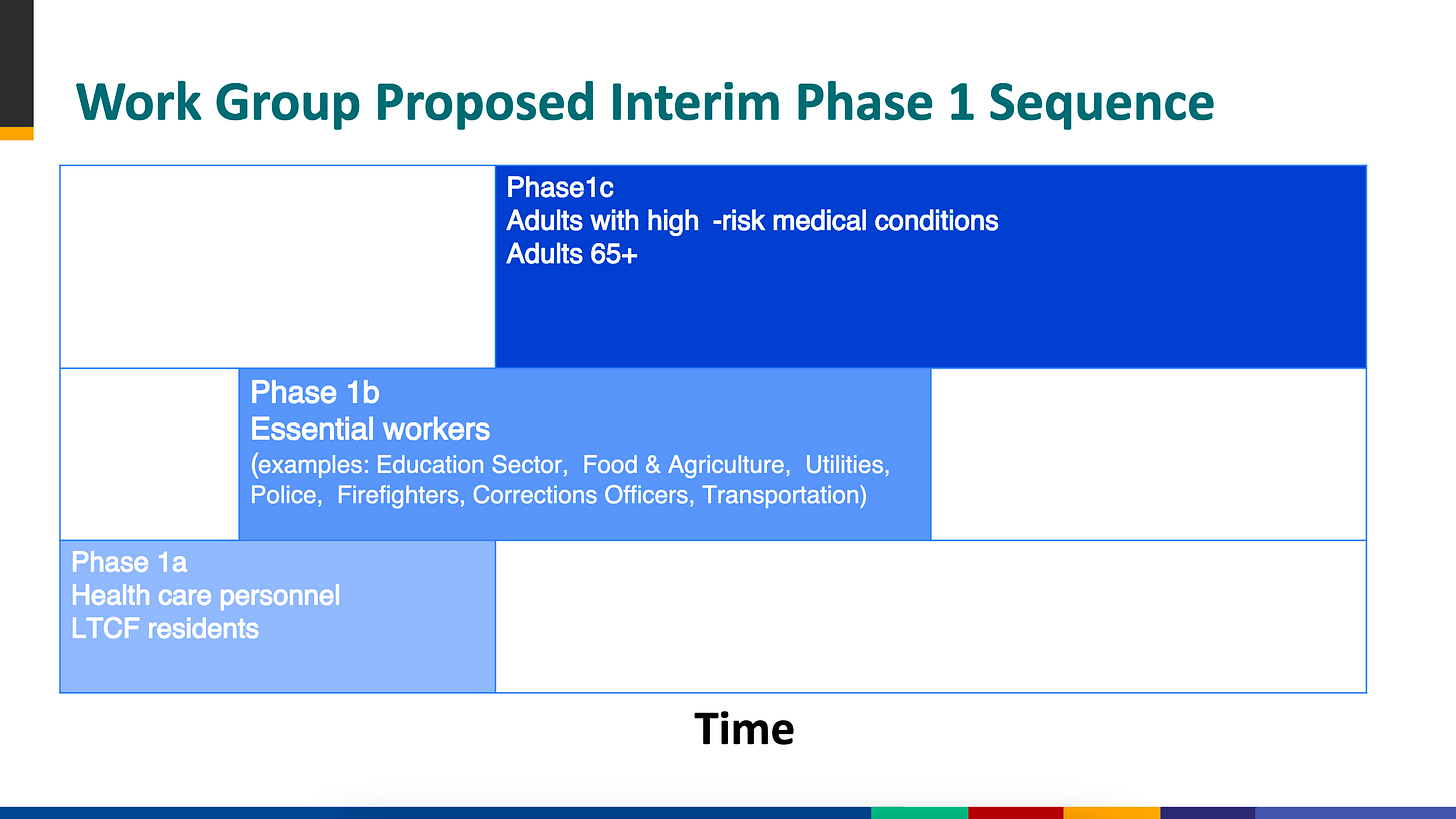
On Tuesday, a working group at the CDC gathered to vote on the group that should receive the first publicly distributed batch of vaccine in phase 1a of the planned roll-out. As expected, the working group voted to prioritize health care workers and adults living in long-term care facilities (a group that includes nursing home residents). This timeline is not binding; ultimately, governors are responsible for deciding the order of vaccination within their states. But it’s unlikely that governors will veer too much from the CDC’s guidelines (probably because no one wants to be the governor telling elderly voters that they won’t get vaccinated first).
Source: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/COVID-02-Dooling.pdf
In all scenarios for how the vaccine is rolled out, though, people under 40 who aren’t health care workers and/or pregnant will get access to the vaccine last.
At the same time, a significant number of millennials and Gen Z’ers will have to be vaccinated for the U.S. to achieve herd immunity and finally curb the spread of COVID-19. This is a big swath of the population that doesn’t really access health care that often—so who will convince them to get the vaccine?
Younger generations and health care
People under 40 (millennials and Gen Z’ers) don’t really access the health care system in the traditional way. Unlike earlier generations that tended to visit single family care physicians for years, millennials and Gen Z’ers switch around frequently and rarely develop a relationship with any one health care worker (except, as I’ll discuss later, perhaps therapists).
Express medical economy
People under 40 are pioneering what I’m calling the express medical economy, a disconnected series of health care professionals, often accessed through an app or online platform, that offer care quickly and in time-bounded interactions. One Medical, for instance, offers primary care from a rotating case of telehealth and in-person providers, frequently offering same-day appointments. Nurx offers online access to birth control; after filling out a questionnaire, a woman can get a prescription that’s been reviewed by an anonymous doctor.
For people under 40, in other words, there’s an entirely new economy of health care, a fragmented patchwork of start-ups with cool brands that treat a variety of different things and don’t necessarily talk to each other, all of which sits almost entirely apart from the traditional system.
There are two general exceptions to this that I can think of, which require regular touchpoints with a single provider or group of providers: 1. gynecological care, and 2. mental health care.
Of course, even in gynecological and mental health care, there are options for an express version of care without relying on any one provider. You can visit a Planned Parenthood or use a service like Nurx for gynecological and family planning services, and you can use an app like Talkspace for mental health care. But I suspect many people still use the traditional medical economy for these services.
The idea of the express medical economy is something I’m still thinking about. It overlaps pretty heavily with the cash-pay industry, which is also growing alongside the traditional system. (This is not unrelated to how intransigent the traditional system is; if you want to build something new in health care, it makes sense to try to go around insurers and other traditional, calcified structures.) If you think I’m missing something, reply to this email or comment below.
But the focus of this email is on the vaccine. Generally, vaccines are messaged and distributed through traditional medical channels. So unless the express medical economy (which is largely online) starts messaging the importance of COVID-19 vaccines, there’s likely to be a big problem with vaccine compliance among people under 40.
CVS MinuteClinic, an example of trade-offs
MinuteClinic started as a series of outpatient, quick-stop treatment clinics in the early 2000s. By 2003, the company had 10 clinic locations in Minnesota. After partnering with CVS in 2005 and then being acquired in 2006, the company exploded. By 2017, there were more than 1,100 CVS MinuteClinics across the country.
MinuteClinic offers very convenient service; for minor illnesses like strep throat, MinuteClinic practitioners can quickly diagnose and prescribe treatment. The services are all in-person, most often within a CVS. If you ignore the fact that CVS is starving out independent pharmacies through shady business tactics, you can relax into the convenience.
But MinuteClinic offered a real challenge to the existing health care system. Its practitioners often have no access to the patient’s medical record, nor do they add entries into a medical record. If a patient has recurrent UTIs, for example, there’s no way to track them or to ensure that the patient isn’t overprescribed antibiotics by a fragmented array of practitioners at multiple different MinuteClinics. And there’s no incentive to get to the root of the recurrent UTIs when Macrobid is $2 and available at the pharmacy counter 5 feet from the clinic. In fact, the American Academy of Pediatrics offered guidance in 2014 strongly recommending parents not use MinuteClinic for their children; the care is just too fragmented.
When it comes to the COVID-19 vaccine, MinuteClinics will be a huge part of the national strategy. They’re on-the-ground clinics with a history of providing other vaccines. But they won’t offer the key factor that longitudinal, traditional care offers—friendly interactions that, over time, build trust. This is the real weakness of the express medical economy, and something that founders and government leaders will have to solve.
Reactive vs. proactive
The lack of regular interactions with the health care system from people under 40 is closely linked to a core problem of the American health system: transitioning care from reactive to proactive.
In other words, most of American health care is provided in response to an acute or chronic problem for which a patient seeks help. And right now, the express medical economy is there to provide time-limited help for that specific problem. But very few start-ups (or doctors more broadly) have the bandwidth to provide preventative care and public health messaging that only bears fruit months or years after the interaction, including messaging on the COVID-19 vaccine.
Conclusion
The COVID-19 pandemic really did the most to expose the worst parts of the American health system. The fragmentation. The structural racism. The expense.
And unfortunately, it looks like the vaccine roll-out is going to do the same. The fragmented express medical economy doesn’t have the built-in relationships that the traditional medical economy offers, and that will probably make it much more difficult to vaccinate people under 40.
But the express medical economy is here to stay, and I suspect more and more people will be transitioning to the ease of use that express and app-based care offers. From a public health perspective, start-up founders, doctors, and government officials need to take that seriously.