Can medicine be over-democratized?
A few startups are prescribing ADHD medications virtually. I think they're going too far.
One of the themes of this newsletter is the idea that virtual care has evolved rapidly in the last few years. The pandemic catalyzed rapid adoption of telehealth, companies stepped in to meet the demand, and the services continue to be popular (albeit at a lower rate than at the height of the pandemic) today.
One topic that I think is still up for debate, though, is when increased democratization of care and greater convenience tips over into potential for poor patient care. One of the most obvious places for abuse is in making potentially habit-forming medications easier to access.
I want to be very careful with this opinion. Sometimes, necessary medications (including potentially habit-forming ones) are rendered inaccessible to people who genuinely need them because of the fear of abuse. And too often, the people who can’t access those drugs are blocked because of their race or gender. This has personally happened to me. The same hospital that gave my teenager brother fentanyl for a Crohn’s flare accused me of being drunk (I was stone-cold sober, which was…easily provable) and refused to give me more than a saline drip for the same kind of flare.
All of that being said, by increasing access to care, telehealth can allow for some sloppy care models that arguably have more potential to do harm than good. Care models that are toggled entirely for access may lack plans for tracking medications and outcomes over time, or easing patients off drugs that are no longer working.
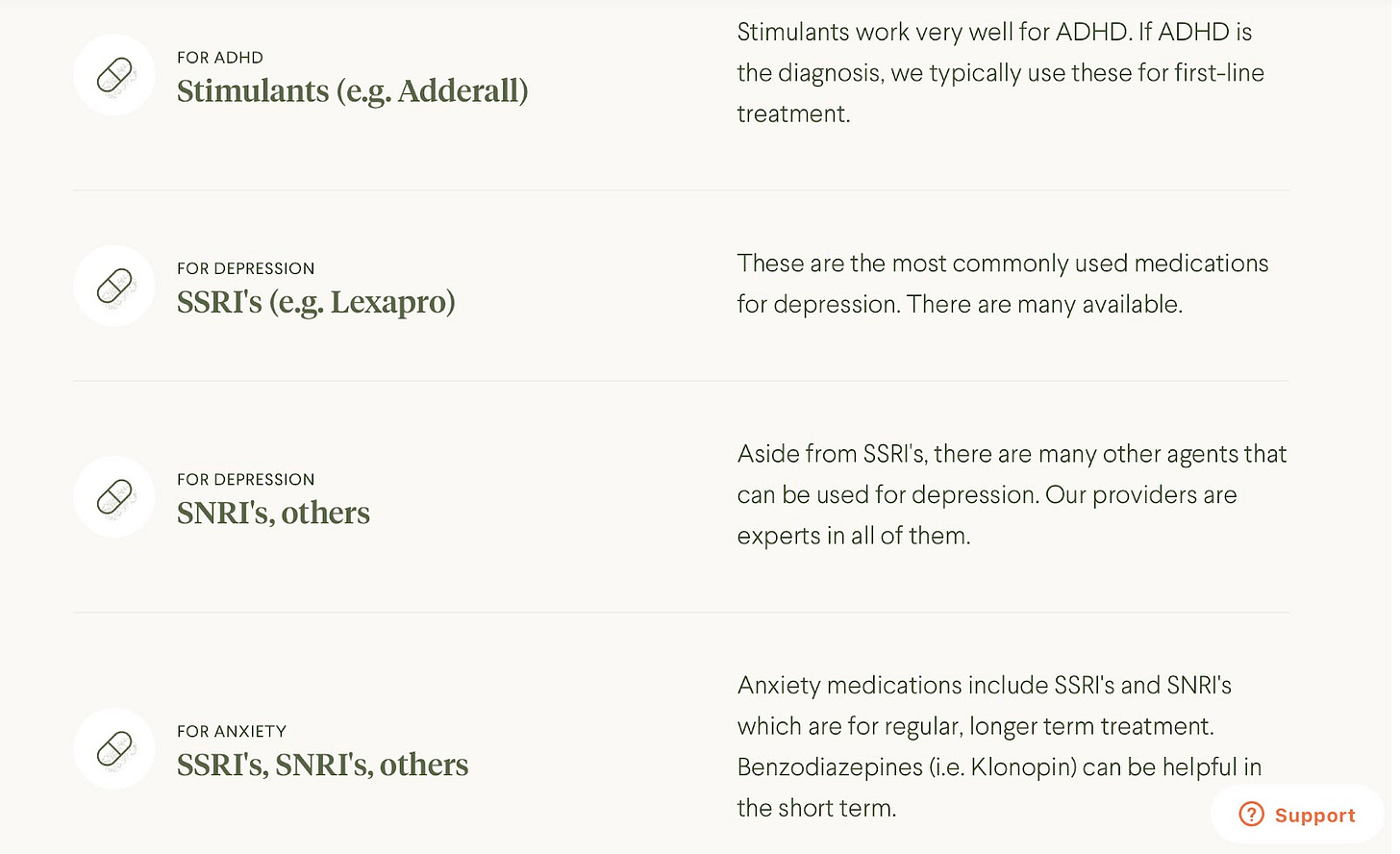
SSRIs change brain chemistry in ways that are not totally known. The medications can increase the risk of suicide, and patients often have to work with their doctors to find the exact right SSRI and dosage. Patients can’t quit suddenly—coming off an SSRI requires a careful taper. And patients who take the medications over a period of years may find that they are stuck in a medication cascade.
Benzodiazepines like Klonopin can be addictive and aren’t indicated for long-term, regular use. Prescription stimulants like Adderall are frequently abused, especially by college students, to get ahead on studying (a non-scientific survey taken by the Michigan Daily in 2018 found that 25% of students were using Adderall to study).
In short, I’m not sure these medications should be readily democratized without much oversight. But it’s happening.
Expanding access to Adderall
As you may have seen in Instagram ads, a few companies have begun to offer ADHD medication and management. From what I can tell (I haven’t personally been a patient), the prescriptions are offered after a short online visit, during which a physician or nurse practitioner (with a valid DEA number, as the job descriptions require) gauges the person’s need for medication and any potential contraindications.
Just two years ago, this process wasn’t legal. The Ryan Haight Act of 2008, passed after a teenager named Ryan Haight died from an overdose of medications purchased online, requires doctors to perform an in-person visit with a patient before prescribing controlled substances. But along with other restrictions loosened by the pandemic, the DEA decided to permit virtual prescription of controlled substances for the duration of the COVID public health emergency (using this decision tree).
Limited oversight
In general, I’m very much in favor of democratizing healthcare access, and I’m in favor of doing it through virtual care models, including condition-specific ones. But the ease of getting prescriptions and the nature of the drugs being prescribed gives me shivers.
For example: When I was researching this piece, I started getting this Google suggestion. (To be clear, this suggestion isn’t any of the companies’ fault—in fact I bet they wish this wasn’t popping up—but to me it is an indicator that people are trying to get a prescription, rather than trying to get care for a condition):
I also found this tweet thread from Will Manidis, the CEO of Science IO, alleging some shady and downright weird behavior from the executive team at Ahead:
It isn’t solely ADHD point-solution companies that are prescribing these medications. Commoditized telehealth platforms also offer appointments with psychiatrists who can easily prescribe similar medications (although general telehealth platforms are less driven by prescriptions and more by visits and PMPM models).
Regardless, many of these companies have yet to answer: Once the patient has the prescription in hand, what oversight is there to ensure the patient takes it as directed and tapers appropriately as needed?
Now what?
I’ve heard no other topic receive so much quiet agreement in healthcare circles than the idea that these companies are pushing drugs with high abuse potential and limited oversight. I’ve also heard speculation that the DEA must plan to rein in these companies soon.
On the other hand, in his end-of-year prediction post, Nikhil Krishnan argued that the Ryan Haight Act might be suspended permanently, given the benefits to people from startups treating substance use disorder (SUD) and prescribing gender-affirming hormone therapy (GAHT).
I wouldn’t be surprised if we see a little of both. The benefits of virtual care models increasing quality access to GAHT and SUD treatment are real. The potential harms of widespread access to drugs with addictive potential seem equally obvious. One outcome could be the DEA interpreting the Ryan Haight Act with more nuance to require follow-up appointments and check-ins, for example.
We’re in the early stages of virtual care, and I have a lot of faith that both startups and legacy providers will figure out high-quality care models for a diverse array of treatment options. Right now, though, I don’t think the care models focused on ADHD medications are hitting the mark.
This information shouldn’t be taken as investment advice (obviously), and the opinions expressed are entirely my own, not representative of my employer or anyone else.





Great article, Olivia! I’ve also heard some arguments similar to this around UTI treatment (typically antibiotics) - it’s become much easier to get a prescription via telehealth but is almost certainly accelerating antibiotic resistance